Matters of Life and Death: Reflections on the Philosophy and Biology of Human Cryopreservation
By Brian Wowk, Ph.D.
The Great Contradiction of Cryonics
Cryopreserving a person for the purpose of future therapy is the distilled essence of cryonics (1). Life or death are not intrinsic to cryonics, except trivially that the purpose of therapy is to save or improve life. There is no therapy for death.
It’s been argued that demonstrably reversible suspended animation, once developed, shouldn’t be classified as cryonics even when used for medical purposes because uncertain outcome is intrinsic to cryonics (2). It’s even been suggested that inability to know whether someone can be revived is a possible definition of death (3). An inability to revive someone can certainly be mistaken for death. However, to categorically call any unconscious person with an uncertain prognosis “dead” would mean that medical intensive care units (ICUs) regularly care for dead people. That would be a contradiction. Unless other lives depend on it, such as an unborn child or organ recipient, medicine doesn’t provide care to dead people.
Even if death isn’t part of the idea of cryonics, the difference between life and death is very relevant to cryonics. Whether death has occurred is relevant to whether there is value in cryopreserving someone. No therapeutic purpose is served by cryopreserving someone who is certainly dead. There is no therapy for death. However, it’s not legally possible to cryopreserve someone who isn’t legally dead. This is the perceived Great Contradiction of contemporary cryonics.
There are two resolutions to the contradiction. The first is semantic, rooted in the meaning of words. The second is biological, rooted in the actual biological state of people cryopreserved under the best conditions that the law allows. It’s not what most people think.
Type I Cryonics
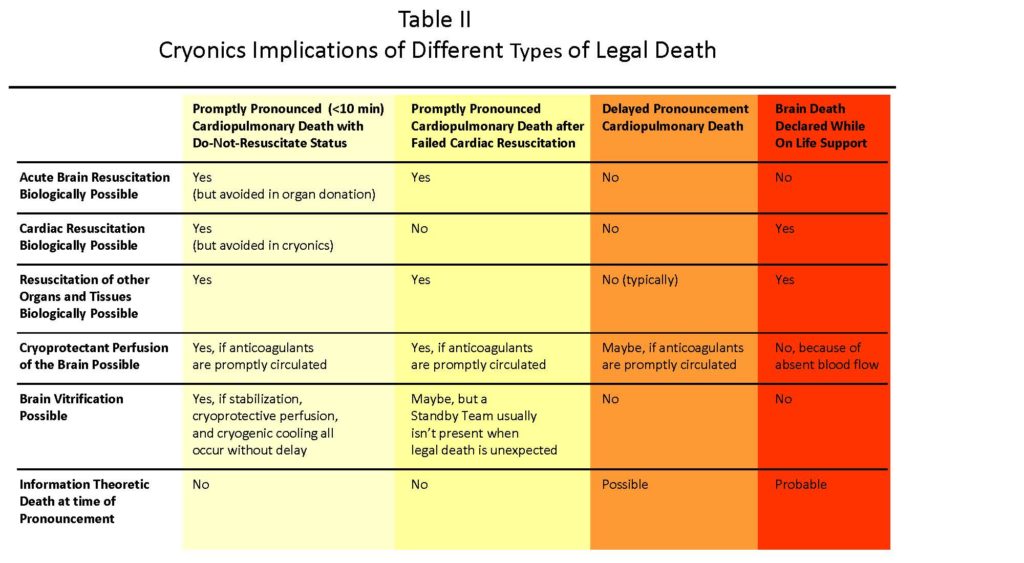
Despite the intention of cryonics to save life, cryonics is often defined as cryopreservation of legally deceased people for the purpose of future revival. However, people who make cryonics arrangements usually envision something more specific. They imagine a team of experts standing by near their bedside (a “standby”) to begin cryonics stabilization procedures as soon as possible after their heart stops beating due to an illness with a predictable course. This is to be followed by successful cryoprotective perfusion and vitrification (ice-free preservation) of the brain, giving the best chance of future revival. The author calls this “Type I” cryonics.
This ideal Type I cryonics is what the scientific case for cryonics is based upon. Studies showing brain structure preservation after cryopreservation usually involve minimal or no circulatory arrest time before cooling and blood substitution begin. Scientists who publicly endorsed a “credible possibility” that contemporary cryopreservation methods might be sufficient to permit future revival in the Scientists Open Letter on Cryonics (4) based that endorsement on “best conditions achievable today.” Demonstrations that wonthe Small Animal and Large Animal Brain Cryopreservation Prizes documenting neural connectome preservation by fixation and vitrification had no circulatory arrest (5-7). The only human cryonics cases that the author is aware of that showed comprehensive brain vitrification by post-cryopreservation CT scanning were begun in Scottsdale, Arizona, near Alcor, with prompt pronouncement of legal death after cardiac arrest (<10 minutes) and a team present to promptly begin stabilization procedures, including artificial restoration of blood circulation.
Type II Cryonics
Cryopreservation of legally deceased people under less-than-ideal conditions encompasses a large universe of possibilities. Possibilities range from delayed pronouncement of legal death (>10 minutes circulatory arrest), a cryonics team not being present (hours of delay), delayed discovery of legal death (days of delay), autopsy before cryopreservation, to even exhumation in very rare cases (8). The author calls human cryopreservation under less-than-ideal conditions “Type II” cryonics.
Type II cryonics occupies a different scientific and ethical space than Type I cryonics (9). While brain cell structure can survive many hours of arrested circulation remarkably well provided that blood circulation isn’t restarted to fuel destructive processes (10,11), blood substitution and cryoprotectant perfusion after long periods of circulatory arrest are usually difficult. Poor cryoprotectant perfusion results in ice crystal formation that may make inferring the original brain cell structure difficult. After many hours of delay, cryoprotectant perfusion may not be possible at all, necessitating so-called “straight freezing” (freezing without cryoprotectant).
Damage to brain cell structure from freezing without cryoprotectant is severe. In worst case scenarios, while one can theoretically describe an atom-by-atom repair process that could reconstitute a healthy brain from any cell debris, like our own brain is built from cell debris of food we eat, it’s difficult to scientifically argue that a brain repaired from some states of damage would still be the original person. A scientific examination of prospects for memory and personality recovery under various damage scenarios is beyond the scope of this article. Suffice to say that the further along the damage spectrum a Type II cryonics case is, the less scientifically defensible cryopreservation is. Type II cryonics does not make good examples for the scientific case for cryonics. Scientific justification for Type II cryonics often rests on plausible deniability of impossibility more than likelihood.
The justification for Type II cryonics is primarily ethical (9). Like comatose patients with an uncertain prognosis in an ICU, the argument for cryopreservation under any conditions that conserve a theoretical possibility of revival is that it’s a conservative thing to do. It defers the decision of whether someone is actually dead (impossible to revive as the original person) for distant future medicine. It could be characterized as a doctrine of “no patient left behind.”
The front-end philosophy of “no patient left behind” could also be applied on the backend. Instead of future medicine pronouncing death when the brain is severely injured, it may be a standard of care for all neurologically injured patients, not just cryonics patients, to undergo whatever degree of molecule, cell, and tissue repairs are necessary to restore healthy personhood even if the result is a second childhood of relearning because most or all original memories were lost (12). Rather than death, social and legal conventions might be, “He lost all his memories and had to relearn everything” (13). Technological repair of severe neurological injury is already of contemporary medical interest (14).
There are practical reasons that it’s difficult to limit cryonics practice to Type I cryonics. Unlike contemporary medical care in which the natural ability to recover homeostasis declines very rapidly after cardiac arrest, there is no obvious point in cryonics practice to “call the code” and consider further cryonics care futile. Cremated remains are certainly past such a point, but 10, 30, or even 60 minutes of cardiac arrest, are almost certainly not. Where should a line be drawn between proceeding or not proceeding with a Type II cryonics case?
This is not to say that Type II cryonics doesn’t itself create ethical dilemmas. If theoretical possibility of revival is to be the justification for proceeding with cryopreservation under poor circumstances, does it not also justify cryopreservation using poor methods (15)? If simple conservation of hope becomes the primary product of cryonics, does this not enable myriad lapses of care, questionable practices, and questionable practitioners all without visible impact? Everybody looks the same under liquid nitrogen.
Type I and Type II cryonics are so ideologically different that there should really be different words for them. It’s an unfortunate reality that most people who make cryonics arrangements hoping for Type I cryonics will legally die under circumstances that make their cryopreservation Type II.
Semantics of Death
Words matter. Choice of words can affect entire outlook on issues. Imprecise use of words can lead to great misunderstanding. For purposes of understanding cryonics, different meanings of the word “death” in different contexts are fraught with layers of complexity.
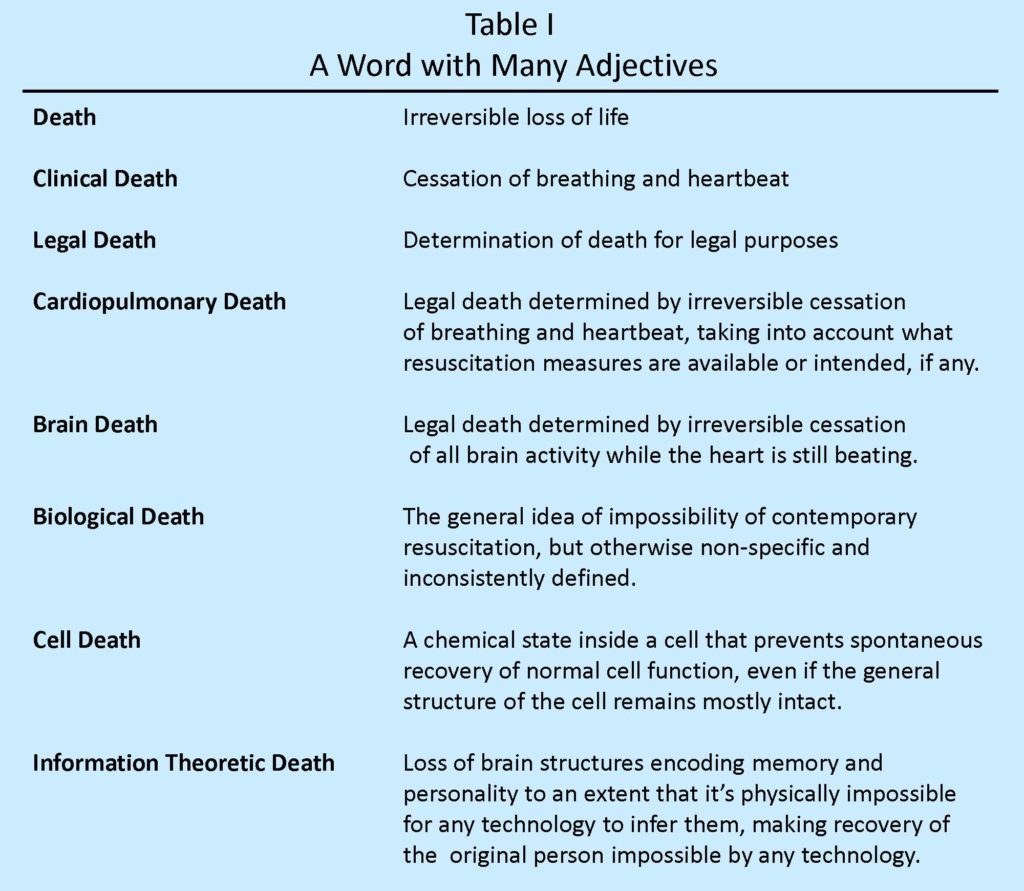
Death is the irreversible loss of life. That’s the usual meaning conjured by the word death. Yet death is also used with a panoply of adjectives that give it different meanings (Table I). Most of these meanings are not consistent with absolutely irreversible loss of life.
The law requires that cryonics patients be legally dead. The law does not require any other adjective, or absence of adjective, denoting absolutely irreversible loss of life. This is the semantic resolution of the perceived Great Contradiction of cryonics. One can be legally dead without being biologically dead, brain dead, information-theoretically dead, or even dead in the plain-language meaning of dead. Legal death is complicated.
Biology of Death
When heartbeat and blood circulation stop at normal body temperature, the ability to restore health in any simple way is lost within minutes. The difficulty of restoring health, or even consciousness, in someone found with stopped blood circulation has made stopped blood circulation (clinical death) practically synonymous with death. We are programmed by culture, law, and even by evolution itself to regard someone with stopped blood circulation as irreversibly lost. They become human remains instead of a human person. The actual biology of what happens when blood circulation stops is much more complicated.
When deprived of oxygen and glucose, normal cell functions diminish or cease. Eventually chemical changes occur inside cells that make spontaneous return to normal cell function impossible even if oxygen and nutrient supplies are restored. This is cell death. Changes to blood and blood vessels can also prevent successful restoration of blood flow in ways specific to different tissues and organs, even if individual cells remain viable. Tendons and skin can remain transplantable for as long as 12 hours after blood circulation stops, limbs for several hours, and organs for tens of minutes, depending on the organ. There is a progression from loss of normal function à loss of ability to recover normal function à dissolution of cell structure. The last step can take many hours, or even days (11).
The long survival of almost all tissue and organs during clinical death is what makes possible reattachment of severed limbs or stopping blood circulation to large volumes of the body for many minutes to surgically repair injuries. While impaired or stopped blood circulation (“ischemia”) starts a cascade of problems that eventually kills everything if the duration is long enough, clinical death is not death.
Biology of Brain Resuscitation
The brain is an extraordinary organ. It uses energy ten times faster per unit mass than the rest of the body. This makes the brain especially vulnerable to loss of blood circulation.
When blood circulation in the brain stops, consciousness is lost in about 10 seconds, and brain electrical activity stops in about 30 seconds (16) resulting in an isoelectric (“flatline”) EEG due to depletion of local energy reserves. Ion pumps in cell membranes stop working. Sodium and calcium ions rush into cells, causing cell swelling, and activation of destructive enzymes and immune-inflammatory processes. Lactic acidosis and a process called excitotoxicity also cause chemical change inside cells (17). None of these processes are immediately destructive or acutely lethal. However, within minutes they can create conditions that doom the brain over hours that follow.
After 10 minutes of clinical death (global cerebral ischemia), the brain exhibits reactive hyperemia (unusually high blood flow) when blood pressure is restored (18). After longer durations of ischemia, an increasing number of brain regions exhibit “no reflow” due to cell swelling acutely blocking microcirculation. After 15 to 60 minutes of restored blood pressure, brain circulation that was hyperemic converts to hypoperfusion (abnormally low blood flow) (18,19). No-reflow areas tend to also convert to hypoperfusion (18), leaving the brain in a state of poor blood circulation for many hours. This recovery period typically occurs in an ICU with a ventilator to support breathing.
Significantly, even for durations of clinical death of 20 minutes, no brain cells actually die, as defined by ability to acutely recover function. Even the most vulnerable neurons in the brain, the CA1 neurons of hippocampus, require hours or days to stop functioning after oxygen is restored, a phenomenon called delayed neural death (20, 21). Some neurons can be recovered and grown under laboratory conditions as long as 8 hours after clinical death that begins at normal body temperature (22, 23). Spontaneous synaptic activity and active metabolism has been observed in brains after restoration of circulation following four hours of normothermic clinical death (24). Why, then, is it so difficult to restore a whole brain to lasting health after mere minutes of stopped blood circulation?
The process of a brain returning to either normal function, or sliding into self-digestion and dissolution after clinical death, happens during hours or days of ICU care following restoration of blood circulation. If brain microcirculation can be restored and maintained after a period of clinical death, and the ion displacements and other disturbances accumulated during circulatory arrest aren’t too severe, then brain recovery can occur. If accumulated chemical disturbances are too severe, then the restored oxygen supply will add free radical damage to other damage mechanisms, and glucose and oxygen will provide the brain with energy that it will use to accelerate its own self destruction during hours that follow. Importantly, brain cell structure persists longer during continuous clinical death than it does if blood circulation is restored after an interval of clinical death that is long enough to prime the brain for self-destruction (10,25).
In the 20th century, 4 to 6 minutes of clinical death at normal body temperature was long enough to set the brain on a course toward self-destruction during later hours of restored blood circulation. In the early 21st century, post-resuscitation therapies, especially mild hypothermia after restoring blood circulation (“targeted temperature management”) allowed brain recovery after longer periods of cardiac arrest than previously thought possible (26-28), even as long as 11 minutes (29) and 16 minutes (30) of complete circulatory arrest at normal body temperature in large animal models with complete neurological recovery.
That cell viability, and especially cell structure, persists for much longer than 10 minutes leaves much room for future improvement of brain resuscitation therapy. That minutes of ischemia only “lights the fuse,” but that it’s actually hours of subsequent blood circulation (or many more hours of absent circulation) that destroys the brain isn’t widely known to non-specialists. However, this two-factor nature of cerebral ischemic injury— an initial ischemic insult followed by reperfusion injury —is now well-established (25,31). In the words of leading experts on brain resuscitation, “Ischemia sets the stage for cellular damage, but it is reperfusion of tissues that generates oxidative stress, creates calcium and pH paradox, and activates an inflammatory cascade that induces cellular death.” (32)
It should be noted that hypothermia during the interval of circulatory arrest slows the rate at which the self-destruction “fuse” is lit by approximately a factor of two for every 10°C temperature reduction (Q10 rule). This is what makes possible deep hypothermic circulatory arrest (DHCA) surgeries in which blood circulation is stopped in the entire body for up to 60 minutes at +18°C. Contrary to popular belief, the record for lowest temperature ever survived by a human isn’t +13°C by Anna Bagenholm during accidental hypothermia and an unknown period of circulatory arrest, but an unnamed female cancer patient at the University of Minnesota who survived a core temperature of +9°C, and 60 minutes of circulatory arrest, in a well-controlled and documented procedure by hypothermia pioneers Suad Niazi and John Lewis in 1955 (33). Recovery after brain inactivation by deep or profound hypothermia and/or circulatory arrest also demonstrates the falsity of the common belief that brain inactivation is synonymous with death.
Brain Death
The advent of life support technology in the mid-20th century led to the observation that sometimes blood flow to brains injured by trauma or ischemia would stop after hours or days of life support. The brain would begin decomposing even if the heart and rest of the body remained functioning. This became called “brain death.” According to the Uniform Declaration of Death Act (UDDA), brain death is one of two methods by which legal death can be declared in the United States. A brain injured by many minutes of stopped blood circulation is a very sick brain. Only much later does it become a dead brain.
Dead While Legally Alive
Brain death is a disaster for cryonics. If allowed to persist for any length of time, it may even be information theoretic death (28,34-36), the total loss of brain information encoding personal identity. Autolytic decomposition of the neocortex can occur even while the brain stem remains functioning on life support. People with cryopreservation arrangements should have an Advance Directive, and an understanding of family members, that they are not to be maintained on a ventilator or other life support if their prognosis for brain recovery is poor.
Cardiopulmonary Death
The other method by which legal death can be pronounced in the United Sates is cardiopulmonary death, defined as “irreversible cessation of circulatory and respiratory functions.” This typically occurs in two different scenarios. In one scenario, after unsuccessful efforts to resuscitate a stopped heart, a physician may “call the code” and pronounce cardiopulmonary death. In another scenario, an aged or seriously ill patient may have an express wish to not be resuscitated if their heart stops beating. Such a do-not-resuscitate (DNR) order means that a medical professional can pronounce cardiopulmonary death upon observed cessation of heartbeat and breathing.
No specific time duration of cardiorespiratory arrest is legally required before legal death can be pronounced for a patient with a DNR status. “Irreversible cessation” doesn’t mean that cardiac arrest be irreversible by any physical means (37-38). It means that cardiac arrest be irreversible in the context of available or planned medical care, which for a DNR patient means no care after cardiac arrest. Since spontaneous return of cardiac function (autoresuscitation) after cardiac arrest caused by pathology is very unlikely, cardiac arrest for a patient with a DNR order is practically irreversible from its onset. Brain death is a biological condition. Cardiopulmonary death is situational, not biological.
Importantly, just as brain death is silent about the condition of the heart, cardiopulmonary death is silent about the condition of the brain. There is no requirement that the brain be dead when legal death by cardiopulmonary criteria is pronounced. Brain death isn’t even clinically defined in absence of blood pressure. Given the complex metabolic activity of dying brains reperfused even hours after clinical death (24), it’s not even clear how brain death could be defined in a cardiopulmonary death context. Cardiopulmonary death is a legal determination by a medical professional that no further care is appropriate for a patient with a stopped heart. That’s all. It’s a formal statement of futility of further care. In the words of one intensive care expert, “Cardiopulmonary death isn’t a diagnosis of death, it’s a prognosis of death.” (39-40).
Alive While Legally Dead
“DONORS AFTER CARDIAC DEATH ARE NOT REALLY DEAD.” This isn’t the raving of a mad cryonics ideologue. This is an all-caps section heading in a mainstream medical journal article discussing cardiopulmonary death in the context of organ donation (37).
Perhaps nowhere is the situational nature of cardiopulmonary death more evident than when CPR is sufficient to maintain consciousness. Normally cardiac output during CPR is insufficient for this. However, in rare instances CPR can keep a patient awake during cardiac arrest (41,42). If the heart can’t be restarted, this can lead to the extraordinary situation of a physician having to “call the code” and cease resuscitation efforts on a patient who is actually awake (43), and with the patient even being made aware that care must cease (44).
Organ Donation after Cardiac Death (DCD)
Most organs donated after legal death are obtained from brain dead donors on life support while the heart is still beating. However in the 1990s a different type of organ donation was developed in which organs are obtained from legally dead donors after cardiopulmonary death instead of brain death. This is called organ donation after cardiac death (DCD). Typically the life of a DCD donor is dependent upon life support, which is removed consistent with prior wishes or family consent. After the heart stops beating, and waiting 2 to 5 minutes (37) depending on institutional policies to ensure cardiac arrest and anesthesia by anoxia, organs are harvested.
Every tissue and organ in a legally-dead DCD donor is still viable when organ harvesting begins, including the brain after only five minutes of ischemia. Even hearts and lungs from DCD donors can resume function in organ recipients. This once again reflects that legal death declared by irreversible cessation of circulatory and respiratory functions is situationally irreversible (45), not physically irreversible.
Legal death in DCD is practically synonymous with legal death in the context of Type I cryonics. The target organs for viable recovery in DCD are transplantable organs. The target organ for viable recovery in cryonics is the brain. The biological resolution of the perceived Great Contradiction of cryonics is that cryonics patients declared legally dead need not be biologically dead.
Like cryonics, DCD highlights legal and ethical issues related to the definition of death. Cryonics has even been brought up in mainstream medical literature debates about DCD (40,46). Debates about when life ends can be as passionate as debates about when life begins, and even more complex. Both debates invoke slippery slopes and sometimes extreme positions. Some might even argue that to fully comply with the Dead Donor Rule ethical principle, no organs should be harvested from anyone until their brain is decomposing, and no cryonics patient should be cryopreserved unless they are brain dead on life support to ensure cerebral autolysis.
Requiring absence of any brain viability would of course be a double standard for legal death because cardiopulmonary death is normally pronounced under much better biological conditions. The issue of a patient being “dead enough” to be moved to a morgue, but not dead enough for a cryonics team to begin stabilization at bedside because of the theoretical possibility of resuscitation was an issue when the hospital was added as a co-defendant in the Roe v Mitchell lawsuit that made California the first jurisdiction to explicitly acknowledge the legality of cryonics (47). The result was a judicial restraining order requiring the hospital to allow application of a portable resuscitator for cryonics stabilization inside the hospital (48,49).
Like debates about the beginning of life, ethical debates about DCD have been about what practice and law should be, not what the law is. DCD ethical debates don’t allege that either DCD organ donation or cryonics stabilization following prompt pronouncement of legal death by cardiopulmonary criteria are illegal, despite the interval of cardiac arrest sometimes being as short as 75 seconds (50). Indeed, a claim that DCD was taking organs from legally living people would be defamation per se against major medical institutions.
Cryonics Stabilization Procedures
The purpose of cryonics stabilization procedures is to stabilize the brain in a biologically viable state before cryopreservation (51). If this isn’t possible, it’s usual cryonics practice to preserve the brain in whatever state it’s found (Type II cryonics). However the purpose of Type I cryonics stabilization is to secure the brain in a biologically viable state as a prelude to cryopreservation. This is true despite prior pronouncement of cardiopulmonary death.
An ideal (Type I) cryonics stabilization requires starting vigorous mechanical chest compressions as soon as possible after legal death is promptly pronounced after cardiac arrest. This artificially reestablishes oxygenated blood circulation to the brain to stop the progression of ischemic injury and accelerate cooling of the brain, while incurring the cost of some reperfusion injury. Medications are administered to inhibit blood clotting, one of which is a calcium chelator that has the side effect of inhibiting cardiac resuscitation. Other chemicals administered by Alcor and its contractors mitigate multiple aspects of reperfusion injury. Blood circulation continues while in an ice bath until metabolism is sufficiently slowed by cooling (Q10 rule) for blood circulation to be safely stopped for surgery to establish extracorporeal perfusion and blood substitution by an oxygenated perfusate as cooling continues.
Reestablishing poor blood flow to the brain after minutes of stopped blood circulation can cause worse reperfusion injury than good blood flow (25). Using vigorous mechanical chest compressions to reestablish blood flow for 30 or 40 minutes of cooling with protective medications to reach +25 degC before stopping for 20 minutes of surgery to access blood vessels is based on the assumption that this results in less damage than keeping blood flow stopped for an extra 20 minutes of +37 degC ischemia to establish extracorporeal perfusion from the very beginning. Such decisions sensitively depend on efficacy of chest compressions, speed of surgery, and future cryonics research.
Brain Function During Cryonics Stabilization
Type I stabilization procedures reestablish oxygenated blood circulation to the brain under conditions compatible with successful contemporary brain resuscitation. That is the intention of stabilization because significant cerebral ischemic injury isn’t empirically compatible with successful vitrification (ice crystal avoidance) of the entire brain. An anesthetic is included in stabilization medications with the dual purpose of reducing brain electrical activity to avoid wasting cell energy that is best used for restoring and maintaining ion homeostasis, and to prevent theoretical possibility of return to consciousness.
More than the briefest intervals of brain ischemia will initially result in coma rather than consciousness upon return of blood circulation (52), even though brain metabolism (O2 consumption, glucose consumption, CO2 production) will proceed apace. Typical acute EEG activity when blood circulation is restored after minutes of brain ischemia is isoelectricity or burst suppression (53), neither of which is compatible with consciousness.
It’s been noted in cryonics case reports (54,55) and mainstream medical literature (46) that respiratory reflexes (agonal gasping) can rarely occur during cryonics stabilization. Does this mean that (a) legal death was improperly pronounced, (b) there is too much blood flow to the brain, or (c) there is too little blood flow to the brain? The answer is actually (c). As discussed, the brain is still biologically viable when legal death is properly pronounced by cardiopulmonary criteria. Neurological responses are to be expected when blood flow is restored, including brain stem function. Agonal gasping (“agonal” in this context referring to end-of-life rather than discomfort) is an unconscious brain stem reflex that can occur with or without chest compressions during cardiac arrest (56) but is more likely after some blood flow is restored to the brain stem by CPR (57). Even though gasping helps improve blood flow, agonal gasping still indicates poor overall brain perfusion. Importantly, an onset of gasping during chest compressions doesn’t indicate cardiac resuscitation.
It’s essential for cryonics caregivers to understand that even after minutes of cardiac arrest and properly-pronounced cardiopulmonary legal death, the brain remains biologically viable. It will neurologically respond to blood flow and treatments the same as the brain of a legally living patient during resuscitative and post-resuscitative care because cardiopulmonary death is a prognosis of brain death, not a diagnosis of brain death (40). The objective of DCD organ donation is to recover biologically viable organs to save the life of a recipient. The objective of cryonics stabilization is to recover a biologically viable brain to save the life of the donor.
Extracorporeal Circulation and Theoretically Ideal Procedures
It’s possible to envision cryopreservation of terminally ill patients someday becoming a legally permitted elective procedure (58). Like deep hypothermic circulatory arrest, a patient would be anesthetized and placed on extracorporeal (heart-lung machine) circulatory support, except there would be no circulatory arrest. Cooling and hemodilution would smoothly proceed to cryoprotectant perfusion and then cryogenic cooling. At the end of the process, the patient would be biologically dead, and therefore legally dead by cardiopulmonary criteria because cryopreservation is presently irreversible. However there would be no clinical death or legal death at the beginning of the procedure, nor any easily-definable point during the procedure that the procedure became irreversible.
The above thought experiment shows that cryonics isn’t intrinsically about cryopreservation of dead people. Cryonics procedures today cannot begin before legal death, cryonics sometimes cryopreserves people who are biologically dead (Type II cryonics), and all contemporary cryopreservation methods assure cardiopulmonary death. However the intention of cryonics isn’t cryopreservation of dead people.
Life or Death
People wake from sleep. People wake from comas. People do not wake from being dead. People wake from being clinically dead, but clinical death isn’t a type of death any more than a Braxton Hicks contraction is labor, or a phantom limb is an appendage. Clinical death looks like death, but not everybody who looks dead is dead.
Nor is legal death a type of death. Like becoming a legal adult or legally married, legal death is a transition of legal status and treatment. However it isn’t a specific biological state or intrinsically indicative of resuscitation potential. Like sunset isn’t night, legal death doesn’t always conform to the ordinary meaning of death (59).
Eventually twilight becomes night. Eventually so much change occurs in a brain after clinical death that no possible technology could revive the original person. The brain information that makes a person unique just won’t be there anymore (information theoretic death). This is the ordinary meaning of the word death—the irreversible loss of a person from this world.
As a practical matter, a person is lost when means to resuscitate them is exhausted or declined. If a clinically dead person has declined resuscitation, then actual death is assured. If resuscitation is attempted, then that same person isn’t dead for practical purposes until resuscitation fails. If acute resuscitation fails and cryopreservation is declined, then death is assured. If there is cryopreservation for future treatment, then that same person isn’t dead for practical purposes until future treatment fails.
Although legally dead, the actual state of health of a cryopreserved person—the state of being or not being –transfers to the judgement of future medicine. Just as when people wake today after decades of coma, if and when cryonics patients wake in the future they will be viewed as having been under care the whole time, not resurrected from the dead (60).
This is an extremely important point. Cryonics looks like interment, but it isn’t. It’s an accepted principle of ethics and common language that someone with an unknown prognosis for regaining consciousness isn’t considered dead until it is known that they aren’t going to wake up anymore.
Whether a particular cryopreserved patient has a chance of being recovered is a matter of opinion. However, once the possibility of recovery is acknowledged (61), then whether that cryonics patient is dead (as distinct from clinically dead or legally dead) is no longer a matter of opinion. It would be an abuse of language to call a potentially recoverable person, especially someone who actually does recover in the future, “dead.”
That potentially-recoverable cryonics patients aren’t dead has both ethical and theological implications. Whether people have souls is a matter of particular religious belief. However if cryonics patients aren’t dead because they are potentially recoverable, then they are still people. If unconscious people have souls, then a recoverable cryonics patient must also still have a soul.
This de-conflation of death with cryonics is crucial for public understanding of the nature and purpose of cryonics. Some religious leaders have explicitly said that cryopreserving people to save life is permissible, but cryopreserving the dead isn’t (62). At the time of writing, more than 80% of the world’s population has religious beliefs about what happens after death that aren’t compatible with recovering dead people from cryopreserved remains. Secularists have their own objections when cryonics is seen as resource-intensive preservation of dead people instead of as a humane extension of emergency medicine (63). This is a major public communications and education issue.
Challenges of Cryonics Regulation
Funeral directors have been integral to the practice of cryonics. They secure death certificates, transit permits, disposition permits, provide transportation arrangements and supplies, host and sometimes assist cryonics teams performing cryonics procedures in mortuary facilities, and work with families for final disposition of any non-cryopreserved remains. As professionals accustomed to accommodating different cultures with sensitivity, funeral directors can be effective facilitators for cryonics practice once needs are explained in detail by cryonics practitioners.
Given the involvement of funeral directors in some aspects of cryonics practice, it may seem that the funeral industry is an appropriate regulatory home for cryonics. However there are serious difficulties with detailed regulation of cryonics by funeral professionals.
The funeral industry deals with human remains on timescales of hours or days. There are no fine distinctions between legal death, biological death, or just death on these timescales. There is no metabolism to support or viability to sustain in mortuary science. There is only supporting final wishes. From a funeral regulatory standpoint, timely transition into liquid nitrogen interment is simply accommodating wishes of particular clients. Biomedical details appear as ritual. Detailed funeral industry regulation of cryonics would be as awkward as funeral directors prescribing to transplant surgeons the timing, methods, and preservation solutions for viable organ retrieval after cardiac arrest, except that cryonics is even more complex.
Imagine if there were regulation of cryonics based only on common knowledge, such as the common “knowledge” that legally dead people are dead. One of the resulting regulations might be a requirement that cryonics companies unequivocally tell people that cryopreservation is only possible if they are dead. Specifying the necessity of legal death before cryopreservation might not be sufficient. Distinctions between legal death and biological death might be seen as misleading. Enforcement might even reach into the websites and publication archives of cryonics organizations to require edits of opinion pieces such as this one. Stranger things have happened.
Regulation based on incomplete understanding can actually inhibit informed consent. For example, if people can’t be told that they are biologically viable during the early stages of cardiopulmonary death, they might not understand that by consenting to cryopreservation they are consenting to partial resuscitative measures that restore blood flow to their biologically living brain. Not being permitted to differentiate between legal death, biological death, cell death, and information theoretic death would also make it impossible to explain the purpose and rationale of cryonics.
This isn’t entirely hypothetical. In response to bad cryonics publicity in 2004, the Arizona State Legislature almost passed a law that would have regulated cryonics in Arizona under the Board of Funeral Directors and Embalmers (64).
Finding appropriate societally-recognized experts to guide cryonics regulation is a difficult problem. Knowledge crucial to cryonics is spread across multiple disciplines including, but not limited to, brain resuscitation, organ cryopreservation, neuroscience, nanoscience and medical futurology. Some of the knowledge is counter-intuitive and contrary to cultural conditioning. Chief among that conditioning is the notion that there is a specific moment of death. In all of science, there is no such moment.
While state-of-the-art cryonics uses tools, knowledge, and often professionals of medicine, cryonics isn’t contemporary medicine. While cryonics sometimes uses funeral professionals, cryonics isn’t mortuary science. Cryonics is something else. Like new adventure sports, cryonics is so small and specialized that the first detailed regulation must likely start from within the field itself.
In the meantime, much of cryonics practice is reliant upon the legal doctrine of nulla poena sine lege (no penalty without law). In other words, an activity is legal unless it’s explicitly illegal, a basic principle of liberal democracy.
It can sometimes be uncomfortable working in a field that lacks the social status and clarity of fine-grained regulation. However that is the very nature of new ideas and practices until they mature. By any measures of social and medical scientific acceptance, cryonics is still very new. If cryonics practice were approached from a philosophy of only doing what permission can be obtained to do, as distinct from doing what isn’t prohibited, the practice of cryonics would grind to a halt. The only place in the world where cryonics was ever ruled explicitly legal, as distinct from implicitly legal, is the State of California (47).
Personnel Working in Cryonics
There are no schools of cryonics, no degrees, no exams, no certifications, no governing professional bodies, and little mentorship. There are only principles, protocols, and standards set by a diminishing number of cerebral resuscitation experts and cryobiologists with personal interest and relevant research experience. This makes cryonics education heavily dependent upon highly self-motivated and curious individuals able to learn by Keller Plan methods. An insatiable appetite for reading large amounts of published information, including historical case reports, followed by interactive questioning of cryonics experts, few that there are, is essential.
Like medical science generally, good stewardship and respect for decades of accumulated written information (libraries) is essential for the health of cryonics as a scholarly science-based practice. Without a foundation of referenceable knowledge, cryonics is a field where it’s easy to assert anything and call it progress. Everybody looks the same under liquid nitrogen.
From time to time there is discussion about whether people working in cryonics need to be “cryonicists,” a cryonicist being defined as someone with personal interest in having their own cryopreservation arrangements. This author believes that two understandings are essential for work affecting cryonics patients. Having a personal interest in cryonics is correlated with these understandings, but being a cryonicist is neither necessary nor sufficient for them.
The first understanding is that a person promptly pronounced legally dead based on cardiac arrest (cardiopulmonary death) is still biologically a living person who will respond to interventions the same as a legally living person undergoing CPR, and who must be cared for by the same thought processes and life-or-death attention to detail as the rescue of a medical patient in cardiac arrest, even though the heart of a cryonics patient will not be resuscitated. This understanding requires considerable biomedical sophistication, but it is a necessary understanding. There are too many examples of poor care resulting from care providers regarding cryonics patients as dead bodies (65) instead of using medical judgement and reasoning appropriate for a biologically functioning patient.
The second understanding is that a cryonics patient must be regarded and cared for as a human person, not human remains, throughout the entire process of cryopreservation and long-term care. This understanding and mindset is necessary even if the prospect for future recovery is believed to be remote. For the general public, whether cryonics patients are people is a matter of opinion. For a cryonics practitioner, regarding cryonics patients as people is a job requirement regardless of personal interest in being cryopreserved. It’s not employment discrimination to require a job to be viewed as saving a life when the job is to save a life. Mindset affects actual care.
Both understandings work together. For example, someone with the first understanding, but not the second, might view cryonics stabilization followed by cryopreservation as improperly ending a life. They might delay or deprioritize stabilization after legal death to expedite biological death before stabilization rather than be involved in care of a biologically living cryonics patient who in their view becomes mere cryopreserved remains. Only if the effect of even a few minutes of ischemic injury on later freezing injury is understood and appreciated as impacting whether a cryopreserved person lives or possibly dies can the “do no harm” ethos of medicine be seen as mandating that cryonics stabilization be begun as early and vigorously as legally possible.
Conversely, someone with the second understanding, but not the first, might regard cryopreservation as a solemn responsibility, but not know how to fulfill that responsibility. Stabilization can’t be properly performed without the understanding that it is stabilization of a biologically living brain. Only with both understandings can the complete process of cryopreservation be understood and performed as a project to save a person’s life.
Informed Consent
Medical patients need not study medicine to benefit from medicine. Medicine rests on a foundation of colleges, medical schools, credentials, licenses, and documented knowledge and traditions of scholarship going back centuries, the products of which are mostly taken for granted. Medicine also has patients who acutely recover, for whom treatment efficacy or lack thereof are obvious.
Cryonics has none of that. Cryonics today is mostly rote application of procedures developed by a small number of scientists working with few colleagues, minimal resources by mainstream standards, and no succession or knowledge perpetuation mechanism other than writing and hope that writings won’t be discarded. The combination of weak knowledge infrastructure and absence of patients who acutely recover (“no feedback” problem) make cryonics very vulnerable to lapsing into procedures and practices that have outward appearances of quality and professionalism, but that may be biologically very poor. There is an ever-present pull in cryonics, like gravity, to count numbers of people cryopreserved, or signed up to be cryopreserved, as primary measures of success.
Cryonics has historically had some protection from this by having a strong “cryo nerd” contingent. A substantial fraction of the early membership of cryonics organizations used to be activists who not only read what their organization published, but who participated as volunteers in cryonics research and cryonics cases. The discipline, or at least the aspiration, of publishing detailed technical cryonics case reports to mitigate the “no feedback” problem of cryonics originated during this era.
With the growth of cryonics, the fraction of people with cryonics arrangements with personal interest in biomedical details is becoming negligible. There’s been an increased focus on streamlining the process of signing up for cryonics arrangements, and moving cryonics information trees deeper into the background. There have even been suggestions to abridge or delete cryonics publication archives, including technical information, based on a rationale that whether to keep any piece of writing on a cryonics website should depend on whether it’s likely to increase or decrease signups. Such information stewardship practices would further erode what little knowledge infrastructure there is in cryonics.
Signing up for cryopreservation after visiting a website that by design and intent purposefully omitted all information that might be dissuasive is practically the definition of lack of informed consent. Yet in cryonics, natural selection favors such websites. There is nothing in cryonics to prevent “the pull of gravity” from evolving such marketing practices other than a cryonics community culture and ethos that shouts down companies that operate that way. Shaming and marginalizing companies that cover cryonics in veneer without substance would be an example of successful cryonics self-regulation.
There are surely limits to how much cryonics can be dumbed down before informed consent is lost. For all the reasons in this article, and many others, those limits are higher than for ordinary medical procedures. Cryonics is contrary to common knowledge almost by definition.
This author believes that informed consent should at least include knowledge that:
* Cryonics isn’t suspended animation; Human cryopreservation presently causes extensive presently-irreversible damage at the molecular, cell, and tissue levels, even fracturing of organs.
* Technologies required for revival are extremely advanced, theoretical, and very distant.
* The prognosis of a cryonics patient depends principally on the condition of the brain.
* Ice-free preservation of the brain is only possible, and still not guaranteed, unless stabilization procedures are begun almost immediately after legal death is promptly pronounced after cardiac arrest, and followed by prompt cryoprotective perfusion and cooling toward liquid nitrogen temperature.
* The risk of legal death occurring under circumstances adverse to quality cryopreservation is very high, and this risk can only be partially mitigated by great logistical efforts.
Crafting biologically and ideologically accurate communications, retaining appropriately trained and motivated personnel, maintaining robust and transparent quality control, navigating and shaping regulation consistent with biologically good care and informed consent, and maintaining the knowledge infrastructure to do it all are among the greatest challenges of cryonics for this century.
Brian Wowk, MSc, PhD is a physicist and cryobiologist specializing in ice-free cryopreservation of organs. He has studied and written about cryonics, medical futurology, and philosophical aspects of death since 1986.
References
- B. Wowk, “Medical Time Travel” in The Scientific Conquest of Death: Essays on Infinite Lifespans, edited by Immortality Institute, pp. 135-150, Libros En Red, 2004.
- T. Donaldson, Neural Archaeology, Cryonics, February (1987) 24-33.
- T. Donaldson, Prospects of a Cure for Death, Cryonics, May (1990) 26-36.
- Scientists Open Letter on Cryonics, retrieved May, 2022, https://www.biostasis.com/scientists-open-letter-on-cryonics/
- R.L. McIntyre, G.M. Fahy, Aldehyde-stabilized cryopreservation, Cryobiology 71 (2015) 448‑458.
- K. Hayworth, The Brain Preservation Technology Prize, Cryonics, 2nd Quarter (2011) 5-9.
- Aldehyde-Stabilized Cryopreservation Wins Final Phase of Brain Preservation Prize, March 13, 2018, retrieved May, 2022, https://www.prweb.com/releases/2018/03/prweb15276833.htm
- Iowa Court of Appeals Upholds Cryopreservation Wishes, Alcor Press Release, May 12, 2010, retrieved May, 2022, https://www.alcor.org/library/iowa-court-of-appeals-upholds-cryopreservation-wishes/
- B. Wowk, Ethics of Non-ideal Cryonics Cases, Cryonics, 4th Quarter (2006) 10-12.
- N.J. Solenski, C.G. diPierro, P.A. Trimmer, A. Kwan, MD, G.A. Helms, Ultrastructural Changes of Neuronal Mitochondria After Transient and Permanent Cerebral Ischemia, Stroke 33 (2002) 816-824.
- A. de Wolf, C. Phaedra, R.M. Perry, M. Maire, Ultrastructural Characterization of Prolonged Normothermic and Cold Cerebral Ischemia in the Adult Rat, Rejuvenation Research 23 (2020), 193-206.
- B. Wowk, The Future of Death, Journal of Critical Care 29 (2014) 1111-1113.
- T. Donaldson, 24th Century Medicine, Cryonics, December (1988) 16-34.
- A.S. Hazell, The Vegetative State and Stem Cells: Therapeutic Considerations, Frontiers in Neurology 7 (2016) 118.
- M. Darwin, The Myth of the Golden Scalpel, Cryonics, January (1986) 15-18.
- R.Pana, L.Hornby, S.D.Shemie, S.Dhanani, J.Teitelbaum,Time to loss of brain function and activity during circulatory arrest, Journal of Critical Care 34 (2016) 77-83.
- R.L. MacDonald, M. Stoodley, Pathophysiology of Cerebral Ischemia, Neurologia Medico-Chirurgica 38 (1998) 1-11.
- E. Kc1gstrom, M. Smith, B.K. Siesjo, Local Cerebral Blood Flow in the Recovery Period Following Complete Cerebral Ischemia in the Rat, Journal of Cerebral Blood Flow and Metabolism 3 (1983) 170-182.
- N.V. Todd, P. Picozzi, H.A. Crockard, R. Russell, Reperfusion After Cerebral Ischemia: Influence of Duration of Ischemia, Stroke 17 (1986) 460-466.
- K. Abe, M. Aoki, J. Kawagoe, T. Yoshida, A. Hattori, K. Kogure and Y. Itoyama, Ischemic Delayed Neuronal Death, Stroke 26 (1995) 1478–1489.
- R. Popovic, R. Liniger, P.E. Bickler, Anesthetics and mild hypothermia similarly prevent hippocampal neuron death in an in vitro model of cerebral ischemia, Anesthesiology 92 (200) 1343–1349.
- R.W.H Verwer, W.T.J.M.C, Hermens, P. Dijkhuizen, O. ter Brake, R.W. Baker, A. Salehi, A.A. Sluiter, J.M Marloes, L.J. Kok, J.V. Muller, J. Verhaagen, D.F. Swaab, Cells in human postmortem brain tissue slices remain alive for several weeks in culture. FASEB J 16 (2002) 54-60.
- S.U. Kim, K.G. Warren, M. Kalia, Tissue culture of adult human neurons, Neuroscience Letters 11 (1979) 137–41.
- Z. Vrselja, S.G. Daniele, J. Silbereis, F. Talpo, Y.M. Morozov, A.M.M. Sousa, B.S. Tanaka, M. Skarica, M. Pletikos, N. Kaur, Z.W. Zhuang, Z.L.R. Alkawadri, A.J. Sinusas, S.R. Latham, S.G. Waxman, N. Sestan, Restoration of brain circulation and cellular functions hours post-mortem, Nature 568 (2019) 336–343.
- D. Crippen, Brain failure and brain death, ACS Surgery: Principles and Practice, WebMD; 2005.
- W.Y. Kim, T.A. Giberson, A. Uber, K. Berg, M.N. Cocchi, M.W. Donnino, Neurologic outcome in comatose patients resuscitated from out-of-hospital cardiac arrest with prolonged downtime and treated with therapeutic hypothermia, Resuscitation 85 (2014) 1042-1046.
- X. Wang, Q. Lin, S. Zhao, S. Lin, F. Chen, Therapeutic benefits of mild hypothermia in patients successfully resuscitated from cardiac arrest: a meta-analysis, World Journal of Emergency Medicine 4 (2013) 260–5.
- Back to Life: The Science of Reviving the Dead, Newsweek, July 22, 2007.
- P. Safar, F. Xiao, A. Radovsky, K. Tanigawa, U. Ebmeyer, N. Bircher, H. Alexander, S.W. Stezoski, Improved Cerebral Resuscitation From Cardiac Arrest in Dogs With Mild Hypothermia Plus Blood Flow Promotion, Stroke 27 (1996) 105-113.
- J. Lemler, S.B. Harris, C. Platt, T.M. Huffman, The arrest of biological time as a bridge to engineered negligible senescence, Annals of the New York Academy of Sciences 1019 (2004) 559-563.
- M.S. Sekhon, P.N. Ainslie, D.E. Griesdale, Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a “two-hit” model, Critical Care 21 (2017) PMC5390465.
- H.B Alam, A.E Pusateri, A. Kindzelski, D. Egan, K. Hoots, M.T. Andrews, P. Rhee, S. Tisherman, K. Mann, J. Vostal, P.M. Kochanek, T. Scalea, V. Deal, F. Sheppard, G. Sopko, HYPOSTAT workshop participants, Hypothermia and hemostasis in severe trauma: A new crossroads workshop report, The Journal of Trauma and Acute Care Surgery 73 (2012) 809-817.
- S.A. Niazi, F.J. Lewis, Profound Hypothermia in Man, Report of a Case, Annals of Surgery 147 (1958) 264-266.
- R.C. Merkle, The technical feasibility of cryonics, Medical Hypotheses 39 (1992) 6–16.
- R.C. Merkle, Molecular Repair of the Brain, Part I, Cryonics, 1st Quarter (1994) 16-30.
- R.C. Merkle, Molecular Repair of the Brain, Part II, Cryonics, 2nd Quarter (1994) 18-30.
- R.M. Sade, Brain Death, Cardiac Death, and the Dead Donor Rule, Journal of the South Carolina Medical Association 107 (2011) 146-149.
- S. Keshavamurthy, P. Rodgers-Fisch, Donation after circulatory death (DCD)—lung procurement, Indian J Thorac Cardiovasc Surg 37 (2021) 425-432.
- B. Wowk, Cardiopulmonary Support in Cryonics, retrieved May, 2022, https://www.alcor.org/library/cardiopulmonary-support-in-cryonics/
- L. Whetstine, S. Streat , M. Darwin, D. Crippen, Pro/con ethics debate: when is dead really dead?, Critical Care 9 (2005) 538–542.
- A. Olaussena, M. Shepherdc, Z. Nehme, K. Smith, S. Bernarde, B. Mitra, Return of consciousness during ongoing cardiopulmonary resuscitation: A systematic review, Resuscitation 86 (2015) 44-48.
- R.L.West, Q. Otto, I.R. Drennan, S. Rudd, B.W. Böttiger, S.Parnia, J. Soar, CPR-related cognitive activity, consciousness, awareness and recall, and its management: A scoping review, Resuscitation Plus 10 (2022) 100241.
- M. Lieber, Patient remains awake for 90 minutes of CPR, doctor says, CNN June 6, 2018.
- During a CPR course in Winnipeg, Canada, circa 1995, the author heard a St. John Ambulance instructor tell an anecdote of care givers at a rural Manitoba hospital being confused by a woman who kept waking during CPR. After cardiac resuscitation was unsuccessful, it was explained to her that CPR must cease.
- Controversies in the Determination of Death, A White Paper by the President’s Council on Bioethics, December 2008, page 84.
- D.W. Crippen, L.M. Whetstine, Ethics review: Dark angels – the problem of death in intensive care, Critical Care 11 (2007) 202.
- C. Mondragon, Big California Legal Victory Affirming the Right to Be Cryopreserved, Cryonics, November (1990) 3-14.
- M. Darwin, Alcor and John Roe Win Temporary Restraining Order, Cryonics, November (1988) 2-6.
- Temporary Restraining Order and Order to Show Cause Re: Preliminary Injunction, Case No. C 697 147, October 28, 1988, retrieved May, 2022, https://www.alcor.org/docs/roe-v-mitchell-tro-28-oct-1988.pdf
- Controversies in the Determination of Death, A White Paper by the President’s Council on Bioethics, December 2008, page 85.
- A. de Wolf, Rapid Stabilization in Human Cryopreservation, 2006, Alcor Life Extension Foundation.
- V. Gorjup, P. Radsel, S.T Kocjancic, D. Erzen, M. Noc, Acute ST-elevation myocardial infarction after successful cardiopulmonary resuscitation, Resuscitation 72 (2007) 379-385.
- M. Dougherty, The Utility of EEG in Prognosis Post-Cardiac Arrest, Practical Neurology, April (2017) 26-27.
- M.G. Darwin, J.D. Leaf, H. Hixon, Neuropreservation of Alcor Patient A-1068, Cryonics, February (1986) 17-32.
- M. Darwin, Cryopreservation Case Report: Arlene Frances Fried, January, 2006, retrieved May, 2022, https://www.alcor.org/library/cryopreservation-case-report-arlene-frances-fried/
- M.S. Eisenberg, Incidence and significance of gasping or agonal respirations in cardiac arrest patients, Current Opinion in Critical Care 12 (2006) 204-206.
- K.G. Lurie, E.C. Nemergut, D. Yannopoulos, M. Sweeney, The Physiology of Cardiopulmonary Resuscitation, Anesthesia and Analgesia 122 (2016) 767-783.
- A. de Wolf, V. Salmensuu, Medical Biostasis Protocol, Biostasis.com, 2020. Also discussed in ADNJ de Grey, Cryonics Takes Another Big Step Toward the Mainstream, Rejuvenation Res. 2020;23(3):191-192
- S.B. Harris, Binary Statutes, Analog World: Burke’s Paradox and the Law, Cryonics, June (1989) 35-46.
- B. Wowk, The Death of Death in Cryonics, Cryonics, June (1988) 30-37.
- R. Freitas Jr., Cryostasis Revival: The Recovery of Cryonics Patients through Nanomedicine, Alcor Life Extension Foundation, 2022
- The author specifically recalls a news story in 2002 in which religious leaders were interviewed in the wake of news reports that Ted Williams had been cryopreserved. The Muslim cleric interviewed said that cryopreserving the dead wouldn’t be permissible, but cryopreservation to save life would be permissible.
- S. Bridge, Has Cryonics Taken the Wrong Path?, Cryonics, February (2014) 22-27.
- Chronology of Attempted 2004 Cryonics Legislation in Arizona, April, 2004, retrieved May, 2022, https://www.alcor.org/library/chronology-of-attempted-2004-cryonics-legislation-in-arizona/
- The author is aware of instances of credentialed medical professionals treating cryonics patients in ways that medical patients would never be treated, including using ice bath water instead of sterile saline to check patency of a parenteral line, using fixed perfusion flow rates during blood substitution without an apparent pressure ceiling, and asserting that blood samples for blood gases or clinical chemistries can’t be acquired or interpreted during cryonics stabilization because “everyone knows that blood can’t be drawn from cadavers.”
